Recent Study Shows How Gut Microbes Can Be Linked To Depression
According to a recent study, microbes that make their home in the gut may have an impact on mental health. According to the most extensive genomic and metabolomic investigation of depression to date, patients with major depressive illness have a distinctive mix of viruses, bacteria, and their metabolic products in their gastrointestinal tracts.
Author:Suleman ShahReviewer:Han JuJul 16, 202360.8K Shares1.1M Views
According to a recent study, microbes that make their home in the gut may have an impact on mental health. According to the most extensive genomic and metabolomic investigation of depression to date, patients with major depressive illness have a distinctive mix of viruses, bacteria, and their metabolic products in their gastrointestinal tracts.
The microbiome of the human gut is a small world occupied by a talkative community of bacteria, viruses, fungus, and protozoa nested inside diverse gastrointestinal niches. Disturbances in this complex microbial civilization have been linked to a number of ailments over the last decade, according to researchers. One such ailment is major depressive disorder (MDD), however investigations have been modest and the results have been ambiguous.
Has The Gut Microbe Been Linked To Depression?
Researchers exploring MDD in the microbiome have been utilizing an inexact approach called 16S ribosomal RNA sequencing, which can only identify bacteria down to the genus level within a batch of microorganisms and excludes viruses. However, psychiatrist Shaohua Hu of China's Zhejiang University School of Medicine and his colleagues wanted a more precise picture of the organisms present, so they collected feces samples from 236 people, half of whom had been diagnosed with MDD and were not on medication, and half of whom were healthy. They sequenced the whole genomic DNA of all the bacteria and viruses in the samples, then compared the differences and similarities between persons with MDD and healthy controls using statistical algorithms.
GABA is a neurotransmitter produced by brain microbes, but it is also produced by gut microbes; MDD patients had lower fecal levels of GABA and certain of its metabolites, and the team discovered that GABA-related microbial genes were altered in MDD patients, suggesting that microbes modulate GABA levels. According to Hu and his colleagues, this may cause a disruption in GABA function in the brain, which could lead to depressed symptoms.
Furthermore, the researchers believe that an increase in Bacteroides bacteria, which produce cytokines, could lead to an increase in inflammation, which has been related to MDD. Reduced Blautia, which has been found to have anti-inflammatory properties, could also have a role in MDD. In other experiments, researchers discovered that transplanting the complete microbiota of a person with MDD into a germ-free rat causes the rat to become melancholy.
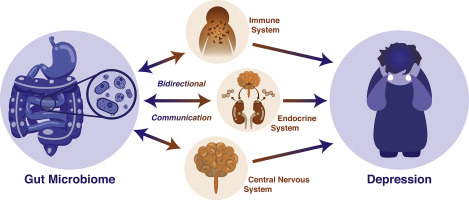
These are speculative claims, and Hu claims that a single cross-sectional study can't prove causality, and instead, "I believe it's a bi-directional axis." Depressed symptoms can affect our eating habits, which in turn can affect our gut characteristics and composition. On the other hand, our bacteria can produce unique chemicals and have a unique pathway that can influence our brain function."
"This sets the stage for a lot more investigation to see if any of these pathways are actually causally associated to depression," adds Cryan, who receives support from Dupont Nutrition, Cremo SA, and Nutricia Danone for his research. "Right now, there's a whole new discipline of nutritional psychiatry growing." Is it possible to target the microbiome with nutrition, and so reduce some of the symptoms of depression?"

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles

