Role Of Left Atrium - How Does It Contribute In Heart Failure?
In the past, the focus on the left ventricle - identified as the only sign and predictor of good or unhealthy cardiac conditions - systematically obscured the role of left atrium.
Author:Suleman ShahReviewer:Han JuJul 28, 20237.1K Shares508K Views

In the past, the focus on the left ventricle - identified as the only sign and predictor of good or unhealthy cardiac conditions - systematically obscured the role of the left atrium.
Recent developments in cardiovascular imaging have offered a greater knowledge of left atrium architecture, physiology, and disease, revealing that this functional structure is far from a passive observer.
The mechanical and neuro-hormonal features of the left atrium are now known to have a role in various cardiovascular disorders, including atrial fibrillation, ischemic heart disease, valvular heart disease, and heart failure.
Heart failure with maintained ejection fraction and decreased left ventricle ejection fraction is linked to anatomical and functional alterations in the left atrium.
Until recently, the left atrium's function in the genesis of heart failure remained unknown. This chamber was assumed to control left ventricle filling and cardiac output in the past.
New non-invasive imaging technologies have increased our knowledge of the left atrium's function and clinical significance.
Furthermore, the left atrium has endocrine and regulatory functions closely tied to its mechanical operation, making it a potential therapeutic target and a predictor of cardiovascular events in various patient groups.
Structure, Function, And Size Of Left Atrium
The measurement of left atrium size is essential for a multiparametric evaluation of heart failure patients. The anteroposterior diameter of the left atrium is assessed using M-mode and two-dimensional transthoracic echocardiography.
However, this is incorrect since the left atrium does not dilate evenly. The maximum left atrial volume indexed to body surface area approach is used since it is thought to be the most accurate.
It is highly linked to cardiac outcomes and allows for risk categorization. The development of three-dimensional echocardiography, which provides a more accurate assessment of the left atrial volume without geometric assumptions and foreshortening, has increased the prediction ability of the left atrial volume index.
The volume measured with cardiac magnetic resonance imaging or cardiac computed tomography correlates better with three-dimensional echocardiography values.
Cardiac magnetic resonance, on the other hand, is regarded as the gold standard in left atrial volume measurement because it offers a sufficient delineation of the inner wall of the endocardium and may identify abnormal features of the myocardial tissues.
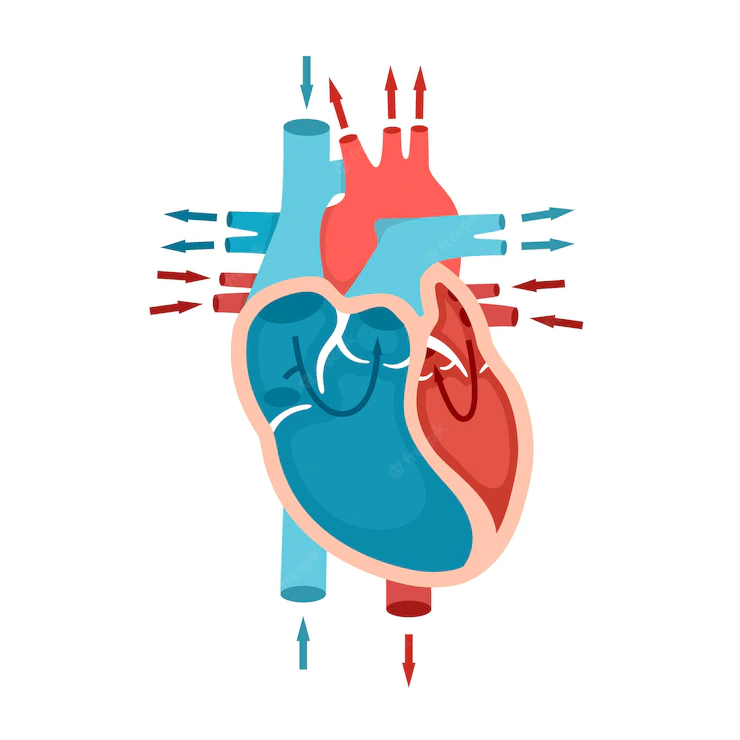
The left atrium is a dynamic structure with three stages of mechanical operation. It serves as a reservoir for oxygenated blood from the pulmonary veins.
Its function depends on the left ventricle filling pressure and the left ventricle end-systolic volume; consequently, any left ventricle dysfunction will affect the atrial reservoir function.
The left atrium is a conduit between the pulmonary veins and the left ventricle during early diastole. The compliance of the atrial and ventricular chambers affects the left atrium's conduit function, which is linked to the reservoir function.
This phase typically contributes just a modest portion of ventricular stroke volume. Still, it predominates in the late stages of diastolic dysfunction when the reservoir function upon atrial contraction is disrupted.
The operation of the atrial booster pump reflects the function of the atrial contractile function. It is determined by intrinsic left atrium contractility, venous return, and left ventricle end-diastolic pressures.
In heart failure patients, there is growing evidence that assessing left atrium function gives more prognostic information than measuring left atrium size. The left atrium function may be evaluated using three-dimensional echocardiography volumetric analysis by measuring all volumes from a single volume trace.
The maximum, lowest, and pre-atrial contraction (just before) volumes may be used to get data on emptying volumes and fractions. Although the transmitral spectral Doppler, pulmonary venous, and left atrial appendix flows indicate phasic function, they are seldom employed.
Tissue Doppler imaging or 2D speckle-tracking echocardiography may also be used to calculate the phasic left atrium function.
2D speckle-tracking echocardiography is the correct approach because it can evaluate myocardial deformation without angle dependence by monitoring the speckle pattern formed by ultrasonic interactions with cardiac tissue.
The left atrium strain measurement is affected by whether the P wave (P-LASr) or the QRS (left atrial strain during reservoir phase, QRS-LASr) complex is utilized as the zero references.
However, a new European Association of Cardiovascular Imaging/American Society of Echocardiography recommendation favors QRS onset as the best approach, owing to the inability to apply the P wave method to all patients, particularly those with atrial fibrillation.
The positive peak of atrial longitudinal strain, which reflects the maximal elongation of the left atrium during the left ventricle systole, determines the reservoir function.
As a result of the interconnectedness of the left atrium and left ventricle chambers, the atrial longitudinal strain peak also reflects the left ventricle's longitudinal contraction.
There is a gradual shortening of the left atrium towards the conclusion of left atrium diastasis until the first negative peak of atrial contraction strain or late diastolic strain. This event represents the operation of the left atrium booster pump.
Remodeling Of The Left Atrium
At least in the early stages of left ventricle diastolic failure, left atrium dilatation is a compensation mechanism necessary to maintain an average stroke volume.
The chronicity and severity of prolonged higher left atrium pressure and left ventricle high filling pressure are reflected in left atrium dilatation.
The Frank-Starling effect improves conduit filling and the first enhancement of its contractile activity. Diastolic property changes enable the left ventricle to function at a greater filling pressure during diastole, increasing the relative contribution of the left atrium booster pump to left ventricle filling until the left atrium preload reserve limitations are met.
The left atrium mainly functions as a conduit during this phase, and mechanical failure occurs. When the left atrium becomes dysfunctional, its buffering role is lost, resulting in pulmonary congestion.
Chronic high-pressure exposure causes structural changes in the left atrium, followed by myocyte hypertrophy, necrosis, apoptosis, and fibrosis. These processes, along with altered ionic channel expression, lead to electrical remodeling and the emergence of atrial fibrillation.
Left atrium dilatation is often accompanied by annular dilatation and the subsequent development of functional mitral regurgitation (MR), leading to pulmonary hemodynamic impairment and heart failure symptoms.
Left atrial volume may also rise in circumstances with normal diastolic function, including bradycardia, high-output states, atrial arrhythmias, and substantial mitral valve dysfunction in trained athletes.
Using left atrium strain as a functional adaptive marker may offer helpful information on left atrium stiffness and an indirect estimate of left ventricle end-diastolic pressure.
It has the potential to detect atrial dysfunction before dilatation begins.
Nonetheless, because of a tight association between the peak of atrial longitudinal strain and left ventricle base downward displacement toward the apex and left ventricle global longitudinal strain, the peak of atrial longitudinal strain should be used with care to diagnose localized left atrium dysfunction.
Pathophysiological Mechanism Of Left Artium In Heart Failure
HFpEF
HFpEF is the most common kind of heart failure in outpatient, accounting for more than half of all decompensated heart failure hospitalizations. It is related to increased morbidity and cardiovascular and non-cardiovascular mortality.
HFpEF, unlike HFrEF, has no definite medications that enhance outcomes. Even in the absence of left atrium enlargement, a 23 percent increase in left atrium reservoir strain was related to a poorer New York Heart Association (NYHA) functional class and an increase in estimated pulmonary capillary wedge pressure (PCWP).
In termsof a historyof atrial fibrillation and past heart failure hospitalizations, a low peak of atrial longitudinal strain score is linked with a greater disease burden.
Investigating left atrium function could result in better treatment management for individuals with suspected or confirmed HFpEF.
HFrEF
The left atrium dimension was a significant predictor of death and hospitalization in studies on left ventricular dysfunction (SOLVD), with 1172 HFrEF patients.
Tissue-Doppler velocity during atrial contraction offers information on the function of the atrial contractile system. This approach is unreliable for measuring left ventricle diastolic pressure combined with left ventricle fibrosis and limited mitral annular motion.
On the other hand, the left ventricle volumetric/mechanical coupling index is a good predictor of mortality and functional mitral regurgitation. Some writers have recommended peak atrial longitudinal strain as a stronger predictor of cardiovascular events than left atrium ejection fraction and left atrium function index.
The lower atrial longitudinal strain values peak was linked to adverse events and heart failure symptoms. The results remained significant even after controlling for B-type natriuretic peptide levels, left atrial volume indexed to the body surface area, E/e' ratio, and left ventricle global longitudinal strain.
In individuals with HFrEF, a lack of reserve in left atrium contractility was related to right ventricular-to-pulmonary uncoupling during exercise and recovery and ventilation inefficiency.
Acute Heart Failure
The peak of atrial longitudinal strain is a robust predictor of outcome in acute heart failure, independent of heart failure phenotype, gender, age, ventricular function, or left atrial volume indexed to the body surface area.
The peak of atrial longitudinal strain is connected with global longitudinal strain at baseline but falls disproportionately with congestion; decongestant treatment is associated with a fast drop in left atrium pressure and quick improvement in reservoir function, regardless of changes in left ventricle global longitudinal strain, left atrial volume, or mitral regurgitation severity.
The significant improvement in the peak of atrial longitudinal strain is associated with a lower likelihood of all-cause or heart failure readmissions. Furthermore, after 6 weeks, the booster pump function restores.
As a result of the concurrent contractile deterioration, this reveals that increased atrial afterload is not the sole mechanism that causes atrial dysfunction.
- Atrial Fibrillation:Heart failure raises the likelihood of developing atrial fibrillation by 10-50 percent in various mechanisms, including intracellular calcium dysregulation, interstitial fibrosis, and autonomic and endocrine dysfunction. Most heart failure patients (regardless of LVEF) have enlarged left atrium and mechanical dysfunction, which lead to pulmonary hypertension and, ultimately, atrial fibrillation development. Age and left atrium dilatation are essential factors in the development of atrial fibrillation.
- Aortic Stenosis:Evaluating left atrium function in individuals with aortic stenosis is gaining popularity. All three left atrium phasic functions in aortic stenosis are much lower than in symptomatic valvular disease. The severity of aortic stenosis and left ventricle diastolic dysfunction is directly connected to left atrium pump performance. The peak atrial longitudinal strain levels of 21% or higher are related to an increased risk of cardiac hospitalization and mortality.
- Mitral Regurgitation:In chronic mitral regurgitation, left atrium dilatation due to volume overload is prevalent and indicates the length of regurgitation and the degree of valvular disease. Atrial function characterization by 2D speckle-tracking echocardiography may provide insights into atrial adaptation to chronic mitral regurgitation. Comparing left atrium function to left atrium size may offer additional information on appropriate surgical time and predict postoperative results.
Left Atrium Therapy In Heart Failure
Because of the left atrium-left ventricle interdependence, lowering left atrium pressure and left atrial volume overload may cause inverse remodeling of the left atrium, resulting in improved ventricular compliance and function.
Reverse remodeling is conceivable after treatment for various illnesses, including mitral regurgitation, atrial fibrillation, and hypertension, as well as cardiac resynchronization therapy.
Cardiac resynchronization therapy may stimulate left atrium reversal remodeling in patients with HFrEF within nine months, increasing reservoir function and left atrium ejection fraction.
People Also Ask
What Is The Role Of The Right Atrium?
The right atrium gets low-oxygen blood from the body and then discharges it into the right ventricle.
What Is The Function Of The Left Atrium And Left Ventricle?
The now oxygen-rich blood from the lungs is received by the left atrium and pumped into the left ventricle.
The left ventricle circulates oxygen-rich blood throughout the body through a vast network of arteries.
Blood pressure is created in the body by the contractions of the left ventricle, the strongest of the four chambers.
What Is The Function Of Left And Right Atrium?
The right atrium gets deoxygenated blood from systemic veins and oxygenated blood from pulmonary veins.
Final Words
Global left atrium failure is linked to an increased risk of incident atrial fibrillation, poor exercise tolerance, morbidity, and death.
Evaluating the left atrium chamber becomes critical for personalized therapy in many clinical circumstances. 2D speckle-tracking echocardiography is a promising approach for quantifying myocardium deformation and providing additional information regarding heart function.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles