How Effective Is The Wide-Awake Approach For Ulnar Nerve Entrapment?
The wide-awake technique for ulnar nerve entrapment offers a unique, patient-friendly solution that reduces the need for sedation and improves recovery times.
Author:Suleman ShahReviewer:Han JuNov 19, 20241.6K Shares233.8K Views

We shall discuss here the wide-awake approach to ulnar nerve entrapment.
The wide-awake approach to hand surgery is gaining increasing popularity worldwide, but PubMedsearch does not reveal any publications on wide-awake ulnar nerve surgery.
In this research study, we describe our surgical experience, techniques, and results of the wide-awake management of ulnar nerve entrapment at both elbow and wrist.
This study is based on a background of having established the world’s first totally one-stop wide-awake (OSWA) hand surgery service, with published outcomes.
Preliminary Discussion
Wide-awake hand surgery enables treatment in one-management stop, through a patient-centric pathway, which is broadly more akin to dental treatment than a traditional multi-stop surgical approach.
The one-stop wide-awake (OSWA)hand surgery service is now well-described in the worldwide published literature.
Wide-awake hand surgery is hand surgery without general anesthesia or regional anesthesia or sedation or tourniquets.
There have been great advances in the technique(s) for hand surgery over the last decade.
It is now over 30 years since the first peer-reviewed publications on wide-awake hand surgery, and despite inherent potential advantages, the worldwide transition to the technique has been slow, according to the published literature.
Some of its probable advantages include:
- lower risk
- a more convenient pathway for the patient
- cost-savings for national state-funded healthcare
The published literature on ulnar nerve compression/decompression reflects that there are two encouraging case series, each comprising 20 cases, which were performed using a local anesthetic technique in 2001 and 1982.
- ulnar nerve and local anesthesia, aka local anesthetic
- wide-awake ulnar nerve
- wide-awake cubital tunnel
- wide-awake ulnar tunnel
- ulnar nerve entrapment
This demonstrates that there has been little recent progress with wide-awake ulnar nerve surgery as would have been expected, despite the recent advances with wide-awake hand surgery.
There is no previous description of an all-encompassing or totally OSWA surgical pathway for the totality of ulnar nerve entrapment, irrespective of site.
The aim of this research study was to discuss the wide-awake approach to ulnar nerve entrapment, which we have pioneered in the U.K.
Materials And Methods
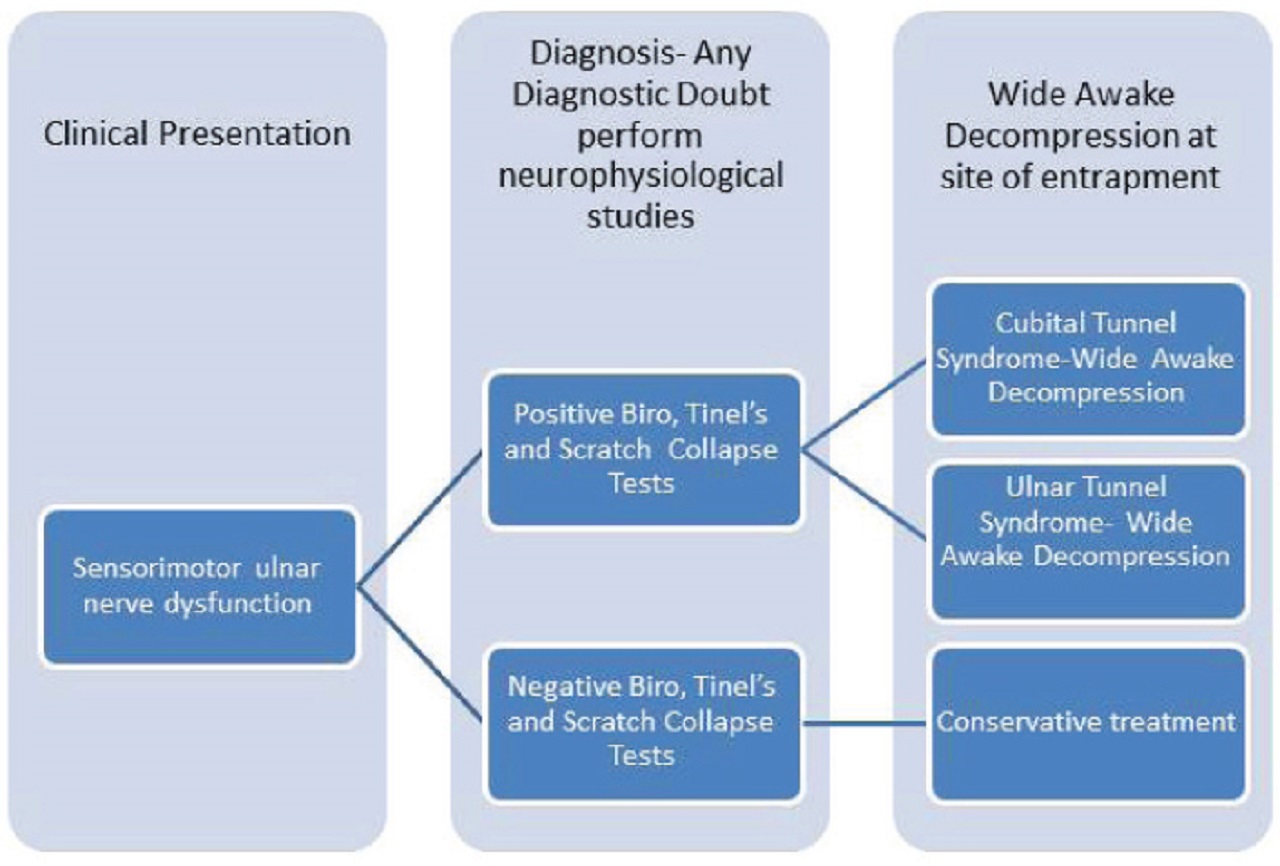
All the patients in this study were managed according to the OSWA ulnar nerve entrapment pathway, with a clinical diagnosis of unilateral isolated ulnar nerve dysfunction (Figure1; see picture below).
Clinical Evaluation
The conduction of clinical evaluation included the following:
b. Biro Test:Sympathetic dysfunction resulted in reduced sweating in little (ulnar nerve) versus index (median nerve) pulp biro slides more easily on affected digits.
c. Scratch Collapse Test:The patient was asked to resist bilateral shoulder external rotation, with the elbows fully flexed.
The area of suspected ulnar nerve compression was then lightly scratched and then resisted shoulder external rotation was immediately repeated.
In ulnar nerve dysfunction, there was momentary loss of shoulder external rotation resistance on the affected side.
d. Tinel’s Test:The ulnar nerve irritability was reproduced by percussion over the cubital or ulnar tunnel.
Surgery was performed under local anesthesia using a lignocaine (lidocaine) and low-dose adrenaline mix, with no tourniquet.
A tourniquet on the upper arm was painful for the wide-awake patient and would encroach upon the surgical field for proximal operations.
In our experience of wide-awake surgery, meticulous dissection enabled surgery without diathermy.
The standard for ulnar nerve surgery was 10 milliliters of 2% lignocaine, with adrenaline 1:200,000, which was drawn up with a 21-gauge needle and infiltrated with a 25-gauge needle.
Cubital Tunnel Decompression Technique (Proximal)
The following steps were followed in this technique:
1. The patient lied down in a supine position.
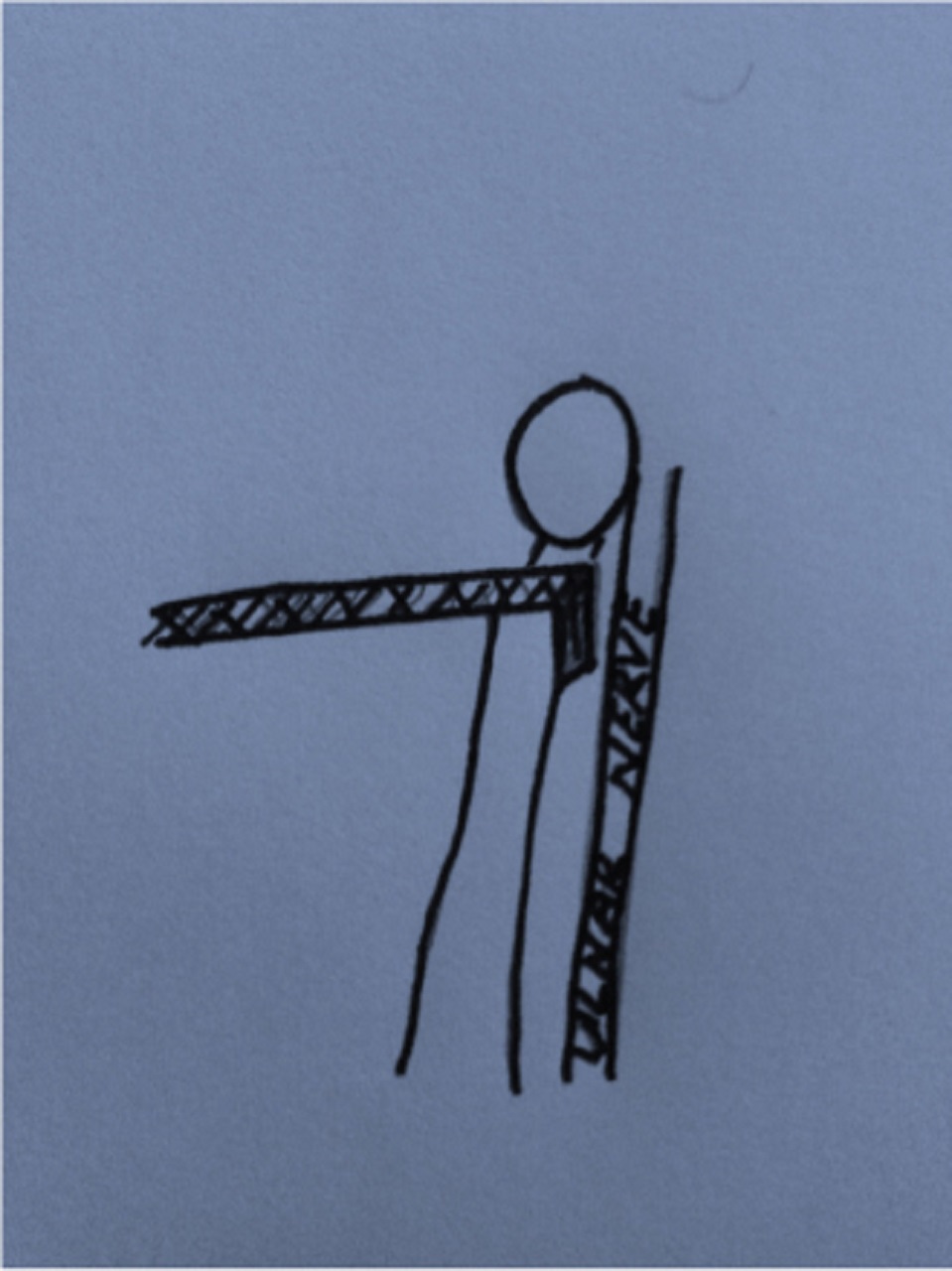
2. Surgical marking positioning was done (see picture below). The picture shows cubital tunnel release positioning.
The following were the findings observed for this surgical mark:
a. Double sandbag was large at base, smaller on top and tucked into the axilla.
b. Shoulder abduction was at 60 degrees.
c. External rotation was maximal.
d. Mark was epicondyle/condyle.
e. Curvilinear incision was guided by palpation of the nerve and in relation to the medial epicondyle.
3. Locate the nerve on the proximal forearm.
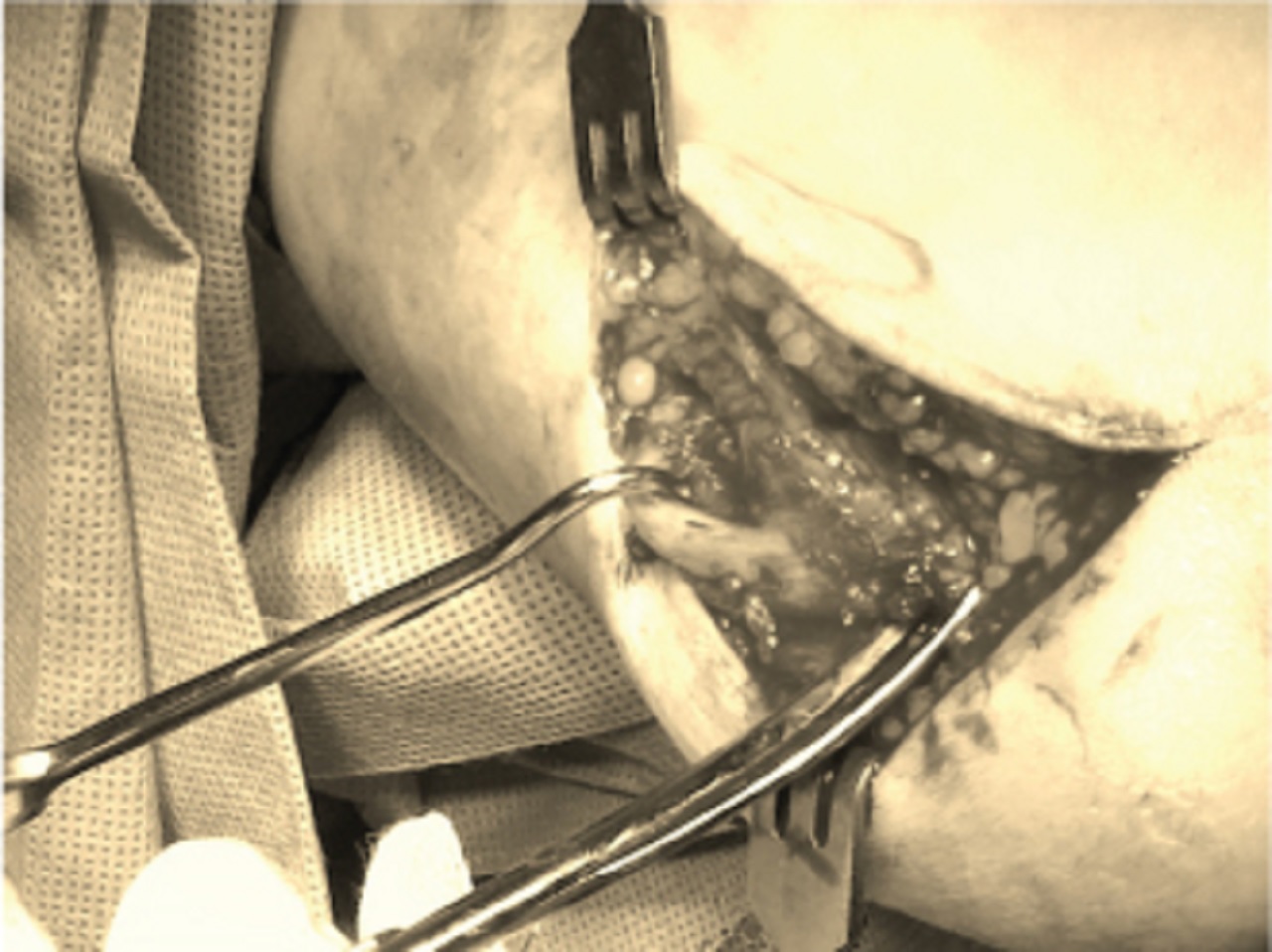
4. Decompress cubital tunnel full-length nerve hook should pass easily around the nerve (see picture below). The picture shows cubital tunnel release intraoperative.
Ulnar Tunnel (Distal) Decompression Technique
The following steps were adhered to in this technique:
1. The patient was positioned supine.
2. Forearm of the patient was supinated on the arm table.
4. Longitudinal incision was made over the FCU (see picture below).
5. Locate the ulnar nerve in relation to the FCU, mobilize the FCU and identify ulnar nerve and protect ulnar artery (see picture below).
6. Decompress the entirety of the ulnar tunnel.
At the OSWA service, we operate continuous audit processes. All patients were requested to contact us immediately in case of any problems.
For the purposes of this audit, all patients were seen once by the orthopedic surgeon in the clinic. Online follow-up was then continued for at least three months post-surgery.
Results Of Wide-Awake Ulnar Nerve Pathway
The protocol for the one-stop wide-awake ulnar nerve pathway is depicted in Figure 1.
There were 40 cases of clinical ulnar nerve compression.
Three injections (mild syndrome as per QuickDASH score) were administered (“DASH” is for “disabilities of the arm, shoulder, and hand”).
Thirty-seven operations (moderate to severe syndrome as per QuickDASH score) were performed, of these:
- three operations were ulnar tunnel decompressions
- 34 operations were cubital tunnel decompressions
The cubital tunnel patients’ diagnoses were made clinically, and the diagnosis was confirmed with nerve conduction studies as required.
The three ulnar tunnel syndrome cases were diagnosed clinically. Two of the ulnar tunnel patients previously had cubital tunnel release, with no improvement.
In addition, there were:
- no intra-operative surgical complications experienced by the patients
- no microbiologically-proven post-operative infections
In all the patients, there were significant subjective and objective improvements in ulnar nerve sensorimotor function post-surgery, including improvements in the validated QuickDASH score.
All the patients were satisfied with the OSWA treatment pathway.
Diagnostic Tests And The OSWA Ulnar Nerve Pathway
The OSWA ulnar nerve pathway is depicted in Figure 1.
All patients were managed to a successful outcome through the OSWA ulnar nerve pathway, and nerve conduction studies did not affect the management.
As part of the informed consent and the discussion of pros and cons and risks and benefits, all the patients were offered electrodiagnostic studies, but in this case series, these tests did not affect the management pathway in any case.
All the patients who had undergone surgical treatment, showed positive:
- Ulnar Biro
- Scratch Collapse Test (SCT)
- Tinel’s test, named after French neurologist Jules Tinel (1879-1952)
In the ulnar tunnel syndrome, there was irritability of the ulnar nerve in the ulnar tunnel rather than in the cubital tunnel, and sensorimotor dysfunction was distal to the site of compression.
Main Discussion
It is now generally accepted that the standard procedure for ulnar nerve entrapment proximally in the cubital tunnel is simple decompression, but more extensive surgery is also described in the literature.
Distal entrapment in the ulnar tunnel is less well described, but in our experience, it is not uncommon, and decompression is the standard surgical procedure.
As per the paper by Elisabet Hagert published in 2012 by the journal HANDon wide awake-treatment of (occult) proximal median nerve entrapment: it is our experience that distal ulnar nerve entrapment may similarly be overlooked and is not usually detected on nerve conduction studies.
Moreover, in the present series, all the three cases of ulnar tunnel syndrome had a false negative nerve conduction study result for ulnar tunnel entrapment, and this has confounded the diagnosis of their clinically obvious ulnar tunnel syndromes.
This underlines the general recognition in the literature that electrophysiology is a possible adjunct to thorough clinical assessment in peripheral nerve entrapment, but that these syndromes are essentially clinical diagnoses.
In this research study, we describe a totally wide-awake approach to ulnar nerve entrapment, irrespective of the site, and all management was performed in one discrete management stop.
The wide-awake hand surgery techniques we utilize enable optimization of patient pathways. Through the wide-awake approach, patients can be safely and effectively treated in:
- one-management stop
- outside the main operating theater
A wide-awake injection technique using epinephrine is now standard worldwide.
A multitude of recent studies have conclusively demonstrated that a wide-awake injection technique using local anesthesia with low-dose epinephrine is safe and effective. This refutes decades of surgical dogma.
The injection technique can be optimized to minimize the associated pain.
The wide-awake approach enables intra-operative optimization, and as described by Michael H. Lavyne, M.D., and William O. Bell, M.D., in their paper published in 1982 by the journal Neurosurgeryand in the original case series of local anesthetic surgery for cubital tunnel syndrome: the usual scenario is an immediate sensorimotor improvement on the surgical table once the complete decompression has been performed.
Feedback from a wide-awake patient can therefore be used to optimize the surgery.
Usually, this is the best guide to ensure that a complete decompression has been performed, but moreover, this can be a guide to fine tune the procedure with techniques, such as epineurotomy.
Conclusion
Wide-Awake Hand Surgery (WAHS) techniques rebalance surgical risk by eliminating the risks of:
- general anesthesia
- regional anesthesia
- sedation
- tourniquets
There is a rebalancing of risk for patients undergoing totally wide-awake ulnar nerve decompression.
The present audit demonstrated that a one-stop wide-awake (OSWA) approach to ulnar nerve entrapment is safe and effective, with high levels of patient satisfaction, and is efficient in terms of processes and cost-savings for state healthcare.
Therefore, the wide-awake approach to ulnar nerve entrapment should get more support.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles