What Are Astrocytes And What Role Do They Play In Intellectual Disabilities?
Astrocytes are the glial cells with the most significant size and the highest density. They are broadly dispersed throughout the brain and are double in the number of neurons.
Author:Suleman ShahReviewer:Han JuJul 18, 202318.9K Shares789.1K Views

Astrocytesare the glial cells with the most significant size and the highest density. They are broadly dispersed throughout the brain and are double in the number of neurons.
Neurological dysfunction is the underlying cause of intellectual disabilities, a neurodevelopmental illness. Their prevalence is strongly related to brain growth.
Astrocytes are crucial to the development of the nervous system. Understanding the astrocyte process in diseases associated with intellectual development disorders can assist in identifying novel therapeutic targets for treating conditions associated with intellectual disabilities.
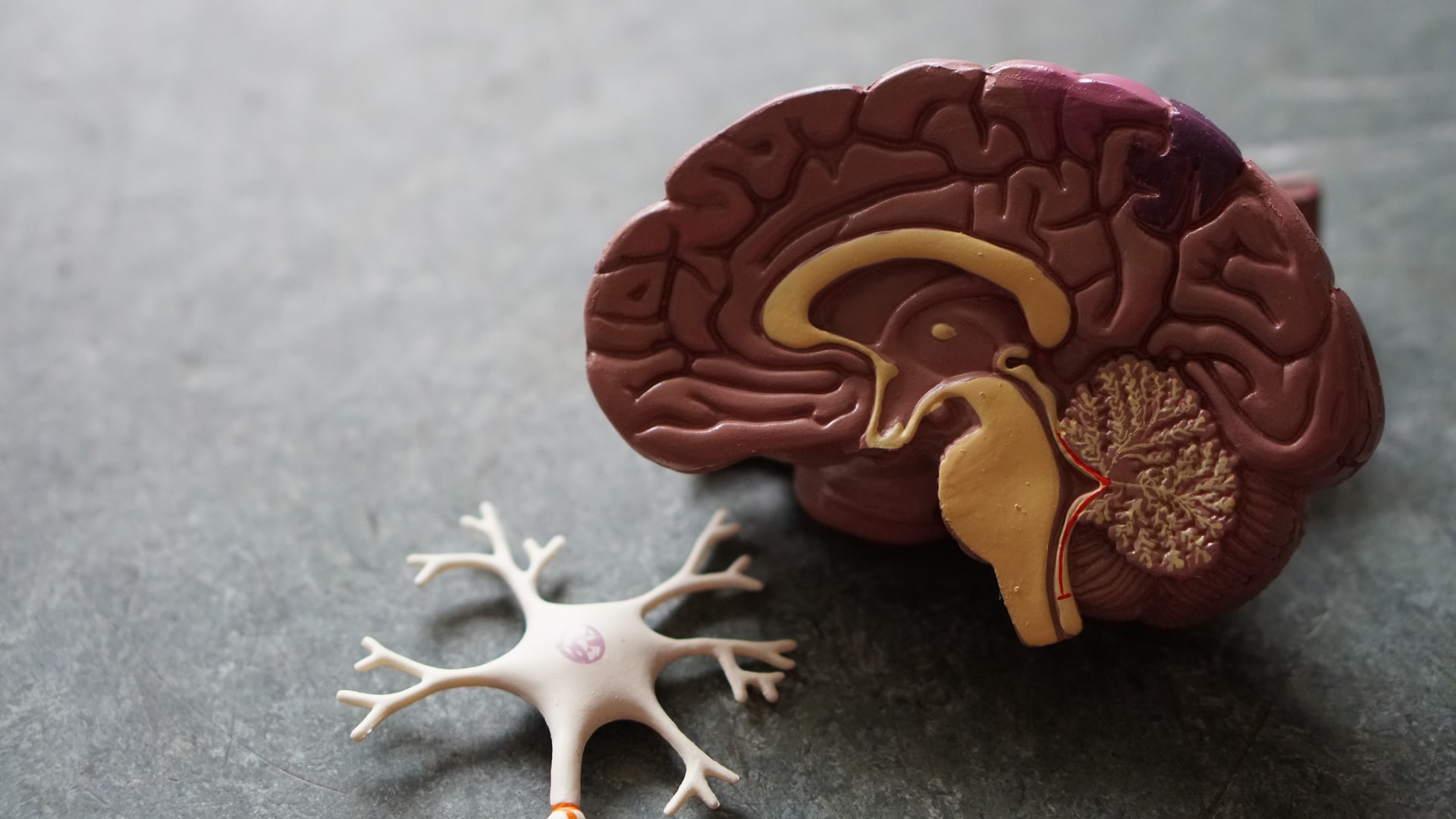
What Are Astrocytes?
Astrocytes are extensively dispersed in the brain and are the most extensive glial cells in size, with a number in the brain more significant than neurons. They are called Astrocytes because they resemble stars.
Astrocytes developed from neural progenitor cells and subsequently differentiated into two kinds of cells depending on their location in the brain: fibrous astrocytes and protoplasmic astrocytes. Fibrous astrocytes are thin cells with few branching found mainly in the white matter of the brain marrow.
Furthermore, fibrous astrocytes contain many glial filaments of glial fibrillary acidic protein (GFAP). Protoplasmic astrocytes, on the other hand, contain more cytoplasmic branches and fewer glial filaments, primarily found in grey matter.
Recent research on single-cell sequencing showed that astrocytes might have numerous subtypes with distinct transcriptome profiles. These brain region-specific subgroups had diverse morphological and physiological roles.
Astrocytes recognize molecular markers. GFAP is an astrocyte-specific molecular marker protein. Because GFAP expression is linked to astrocyte activation, it may be employed as a reliable and sensitive marker of reactive astrocytes.
These molecular markers offer an essential foundation for studying astrocyte functions and alterations in the diseased condition of the central nervous system.
What Are Astrocytes?
What Is Intellectual Disability?
Intellectual impairment is a neurodevelopmental disorder defined by intellectual function and adaptation deficits that often emerge during the formative phases. It is the most prevalent symptom of numerous diseases, including Rett syndrome, Down syndrome, and fragile X syndrome.
Patients with intellectual disabilities have an overall cognitive quotient of < 70. The primary cause of intellectual impairment is neuron growth retardation. Previous research suggested that neuronal architecture and functional alterations contribute to intellectual impairment.
Astrocytes have been discovered to have an essential role in impacting the function of brain development in recent years, thanks to ongoing research on astrocytes. The findings of gene sequencing in intellectually disabled individuals demonstrate that a high number of intellectual disability-related genes are mainly expressed in astrocytes rather than neurons, indicating that astrocytes, like neurons, are essential intellectual disability regulators.
Astrocytes Functions
Astrocytes form mostly surrounding neurons, and their processes may expand and fill the cell body and neurite to support and separate the neurons. The end process of specific astrocytes forms the end foot, making it easier to stick to the capillary wall or the brain and spinal cord surfaces to create glial-limiting membranes.
Astrocytes have been discovered to control the central nervous system via ongoing research. Astrocytes may communicate with neurons in two directions, contribute to synaptic composition, respond to neurotransmitters generated by synapses, and become reactive in response to chemical or physical injury.
They may also be triggered by microglia and govern the death of neurons and oligodendrocytes. These reactive astrocytes are also involved in synapse production, clearance, and control of synaptic plasticity.
Furthermore, astrocyte ion channels metabolize neurotransmitters and ions such as glutamate and adenosine triphosphate (ATP), control neuronal excitability, and maintain the blood-brain barrier.
These findings suggest that reactive astrocytes play a complex role in the etiology of intellectual disability. The purpose of this mini-review was to explore the morphological and functional alterations of reactive astrocytes in intellectual disability-related disorders, as well as to address the potential effects of medications on the astrocytes.
Role Of Astrocytes In Intellectual Disability
Both genetic and environmental causes may cause intellectual disabilities. In termsof genetic factors, Down’s syndrome is caused by chromosomal variation, Williams syndrome is caused by deletion of the region near the long-arm chromosome 7, Fragile X syndrome is caused by FMR1 gene defect and protein product deletion, Rett syndrome is caused by the MECP2 gene mutation on the X chromosome, and Tuberous sclerosis (TS) caused by TSC1 and TSC2 gene mutations can all result in intellectual disability.
Regarding environmental variables, hunger, brain trauma, maternal, perinatal infection, and early childhood central nervous system illness have all been linked to intellectual disability.
Neuronal alterations are the source of many hereditary diseases, including Down’s and Fragile X syndrome. The pathogenic involvement of astrocytes in neurodevelopmental disorders has been well investigated, indicating that alterations in astrocytes may play an essential role in the pathogenesis of intellectual disability.
The importance of astrocyte morphological and functional abnormalities to the emergence of intellectual disability eventually emerged from an in-depth research of the morphology and function of glial cells.
Reactive Astrocytes
When the central nervous system is injured, or pathological changes occur, astrocytes respond to aberrant nerve cells by releasing various chemicals both within and outside the cells, resulting in haemostatic, morphological, and functional abnormalities and the transformation of reactive astrocytes.
Increased reactive astrocytes will have beneficial or detrimental effects on peripheral nerve and non-nerve cells through available alterations. Reactive astrocytes will vary with the severity of nervous system damage. Increased reactive astrocytes are widespread in all central nervous system injuries and are often recognized as pathological signs of central nervous system injuries. Pathologically, activated astrocyte markers such as GFAP and S100 were also elevated.
GFAP and S100 levels were likewise elevated in astrocytes from numerous neurological illness models with cognitive impairment symptoms, including Rett syndrome, Down’s syndrome, fragile X syndrome, and Tuberous sclerosis, demonstrating that reactive astrocytes are considerably elevated in intellectual disability-related disorders.
Increased reactive astrocytes in intellectual disability-related diseases have typically negative consequences on the central nervous system, which is evident in the inflammatory response.
Inflammatory factor expression levels, such as IL-1, IL-6, and TNF-, were upregulated in Rett syndrome astrocytes, TNFR2 expression was significantly increased in fragile X syndrome astrocytes, and increased expression of immune response regulators miR-146 and miR-155 associated with the inflammatory response in reactive astrocytes was also observed in a Down’s syndrome mouse model.
The inflammatory response caused by these reactive astrocytes disrupts central nervous system homeostasis by preventing normal neuron development or death.
Astrocytes Ion Channel Dysfunction
Aside from the inflammatory response, astrocytes play a significant role in neuronal ion homeostasis in various intellectual disability-related disorders. The expression of K channels and other ion channels is decreased in the tuberous sclerosis model, reducing their capacity to buffer potassium.
A succession of events will ultimately lead to neuronal overexcitation, resulting in the Tuberous sclerosis complex. Neurodevelopmental impairment and intellectual disability were caused by astrocyte ion channels such as the K+ channel, BEST-1, and hemichannels. Neurotoxicity results from a glutamate/GABA imbalance in fragile X syndrome astrocytes, shortening neuronal dendritic lengths.
The tuberous sclerosis model also reduced the expression of glutamate transporters such as GLAST and GLAST. Metabotropic glutamate receptor 5 expression and Ca2+ response were reduced in the Rett syndrome model, decreasing the expression of neuron-dependent GLT1 and subsequently limiting neuronal glutamate uptake.
Excitotoxicity causes central nerve cell death and decreased synaptic plasticity and learning when extracellular glutamate levels rise. Research on illness models has shown that reactive astrocytes may also protect neurons from injury to the central nervous system.
Astrocytes Molecular Dysfunction
Changes in reactive astrocyte molecular pathways are also prevalent. Many proteins' expression levels in astrocytes of different disorders will also influence their incidence. Reduced brain-derived neurotrophic factor (BDNF) may be one of the causes of aberrant neural development in the Rett syndrome model.
Sustained high S100 expression in astrocytes increases the generation of reactive oxygen species and activates the stress response kinase, resulting in cell death in the Down's syndrome model. Coculture reduces the quantity of calcium-binding presynaptic proteins, synaptophysins, and postsynaptic scaffold proteins, PSD95, at neuronal synapses, resulting in aberrant dendritic architecture.
Dysfunction Of Astrocytes In Environmental Factor-Associated Intellectual Disability
Excessive alcohol use as a result of environmental circumstances will also have an impact on the process of intellectual growth. Ethanol has been shown to reduce total protein in astrocytes and inhibit astrocyte serotonin absorption. This research sheds light on the link between ethanol and CNS development.
A pregnancy-related infection will also have an impact on astrocyte and neuron development. The disease affected astrocytic biology and increased the number of reactive astrocytes. The offspring of rats infected during pregnancy have increased serotonin receptor sensitivity, raising the risk of neurological disorders.
The expression of GFAP and IL-6 was elevated in the astrocytes of rat offspring infected during pregnancy, resulting in aberrant myelin formation. Infection during pregnancy harms brain development, resulting in intellectual impairment and neurodegenerative illnesses, which may be the primary molecular causes of intellectual impairment caused by pregnancy-related infection.
Pb may stimulate astrocytes, causing them to produce inflammatory chemicals and elicit an inflammatory response. Pb may also cause oxidative stress in astrocytes, disrupt the astrocyte cell cycle, promote astrocyte death, and finally lead to neurological disorders. Furthermore, studies have shown that Pb might lower serotonin levels in the mouse brain, contributing to intellectual disability.
Intellectual Disability Of Drugs And Astrocytes
Several medications, including piracetam, aniracetam, monosialotetrahexosylganglioside sodium (GM1), mecobalamin, vitamin B12, and methylphenidate hydrochloride, have previously been used to treat mental illnesses.
Cetam medicines may counteract scopolamine's effects on glucose consumption in the cerebral cortex. Piracetam therapyincreased mitochondrial ATP generation and membrane potential in an Alzheimer's disease model.
GM1 (monosialotetrahexosylganglioside sodium) may inhibit the aberrant release or reuptake of excitatory amino acid neurotransmitters like glutamate. GM1 can also enhance cerebral blood circulation and oxygen levels in the blood and preserve neurons.
Nerve growth requires vitamin B12. Reactive astrocytes were seen in higher numbers in the grey matter of vitamin B-deficient rats with microglial edema and myelinolytic lesions.
Mecobalamin and vitamin B12 may supplement vitamin B12 in the brain, stimulate nucleic acid and protein synthesis, improve axonal transport, regeneration, and myelin formation to avoid axonal degeneration, heal injured nerve tissues, and improve damaged glial cells in the brain.
People Also Ask
What Do Astrocytes Do?
Astrocytes not only control blood flow but also transport mitochondria to neurons and provide the building blocks for neurotransmitters, which power neuronal metabolism. Furthermore, astrocytes can phagocytose synapses, modify neurotrophin production, and remove debris.
What Is One Disease That Astrocytes May Be Related To?
Astrocytes are involved in neurodegenerative illnesses such as Huntington's disease, Parkinson's disease, Alzheimer's disease, and amyotrophic lateral sclerosis.
Do Astrocytes Play A Role In Intellectual Disabilities?
Genetic investigations of intellectual disabilities have shown that astrocytes may play a role in the pathogenesis of these illnesses.
Conclusion
Astrocytes' functions in cerebral development have been steadily studied in recent years via in-depth research. Their alterations are also linked to the onset and course of numerous neurological disorders. The etiology of intellectual impairment is complicated, with various processes yet unknown.
This mini-review demonstrates that functional alterations in astrocytes caused by numerous pathogenic causes are strongly associated with intellectual disability. Many medications used to treat intellectual disability may also reduce astrocyte lesions to variable degrees.
However, a few effective medicines for functional alterations of astrocytes under pathological settings have been used to treat intellectual disability-related disorders. One of the critical mechanisms of these disorders may be morphological and functional alterations in astrocytes.
Dissecting the role of different astrocyte subtypes in intellectual disability-related diseases might lead to a new treatment strategy that would assist these individuals. As a result, medicines that suppress astrocyte lesions can potentially become a novel and essential therapy option for intellectual impairment.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles