Osteopenia - A Marker Of Low Bone Mass And Fracture Risk
Arm yourself with knowledge about osteopenia, the precursor to osteoporosis. Discover its significance as an early warning sign for low bone mass and fracture risk.
Author:Suleman ShahReviewer:Han JuJan 19, 20242.5K Shares318.9K Views
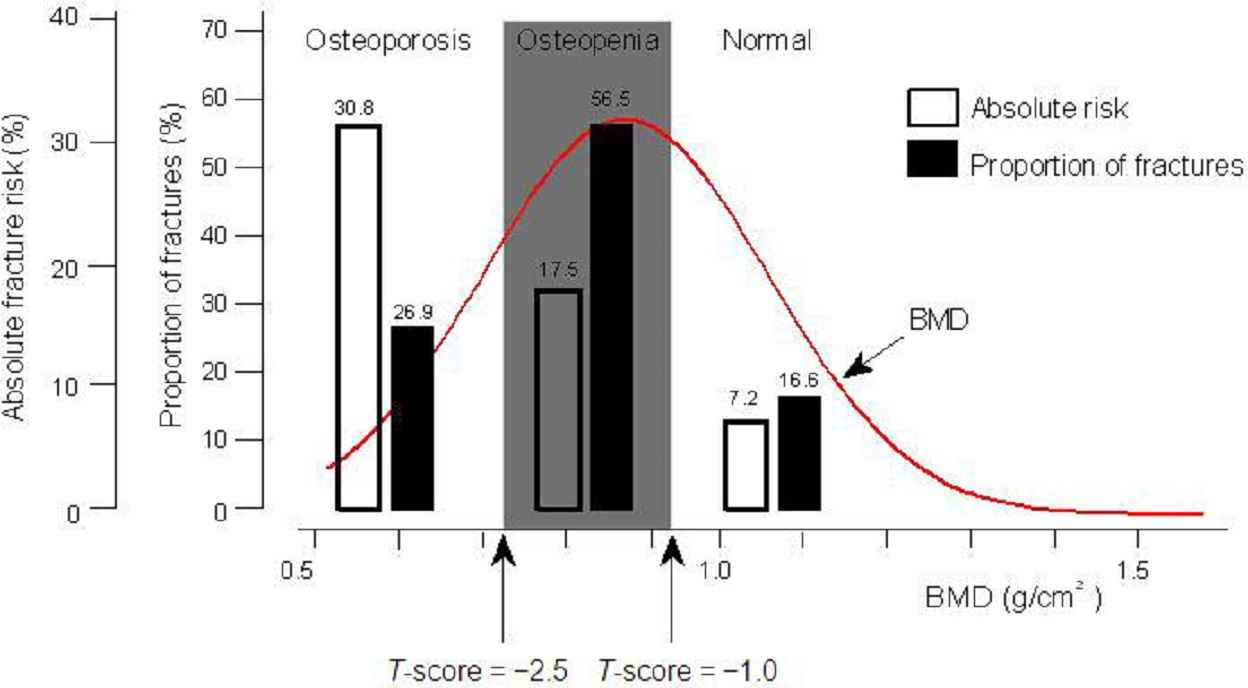
Absolute fracture risk is greatest for individuals with osteoporosis, more than half of these fractures arise from those with osteopenia and normal bone mineral density, a probable consequence of greater numbers at risk in these categories.
However, areal bone mineral density measurements used commonly in clinical practice do not detect differences in bone tissue properties, geometry and microarchitecture, which contribute to bone strength.
Defining Osteopenia And Osteoporosis
For nearly three decades, areal bone mineral density (BMD) has been measured using either dual-photon absorptiometry or, more recently, dual-energy X-ray absorptiometry (DXA) as a marker of osteoporosis.
DXA-derived BMD is calculated as the bone mineral content divided by the area of bone scanned.
This two-dimensional representation of volumetric BMD is confounded by bone size and shape.
Nonetheless, fracture risk increases with decreasing BMD, such that each standard deviation decrease in BMD is associated with a 1.5 to 3.0-fold increase in age-adjusted fracture risk.
BMD is a continuous variable, which approximates a normal distribution.
Based on nominal thresholds recommended by an expert panel of the World Health Organization, BMD is commonly categorized into:
- normal BMD
- osteopenia
- osteoporosis
Osteopenia is the low bone mass category defined by BMD T-scores between negative 1.0 and negative 2.5.
Using these cut-points, 16% of young normal women are defined as having osteopenia and 5% have osteoporosis, but these individuals may make little, if any, contribution to the population burden fragility fracture.
The osteopenia threshold was based on data that derived a theoretical fracture threshold, whereas the osteoporosis threshold was based on the prevalence of fracture among postmenopausal Caucasian women.
Although these thresholds were devised for epidemiological purposes appropriate for Caucasian women, they have been widely adopted for clinical use in broader populations.
Almost half of women aged 50 years and older in Australia have osteopenia (and 23% have osteoporosis corresponding to BMD T-score less than or equal to negative 2.5).
Although thresholds for describing men with normal BMD, osteopenia and osteoporosis have not been defined, the gradient for fracture risk is similar for each standard deviation deficit in BMD for both sexes.
Utilizing similar T-score thresholds for men aged 50 years and older indicates that just over half have osteopenia corresponding to BMD T-score from negative 1.0 to negative 2.5 (and 6% have osteoporosis, T-score less than or equal to negative 2.5).
As there is discordance in BMD between skeletal sites, such estimates depend on the site scanned, as well as the reference range used to determine T-scores.
However, while osteoporosis confers the greatest risk for fracture, fracture risk is not negligible in persons with more moderate deficits in BMD.
Age-standardized 5-year absolute fracture risk derived from total hip BMD at baseline for postmenopausal women in Australia are:
- 30.8% (95%CI 22.0 to 39.6) for women with osteoporosis
- 17.5% (95%CI 13.2 to 21.7) for women with osteopenia
- 7.2% (95%CI 3.7 to 10.7) for women with normal BMD
The aim of this critical review was to explore osteopenia as a marker of low bone mass and fracture risk.
Fracture And BMD
Population-based studies reveal that the burden of fracture arises, not from the relatively small, high-risk group with osteoporosis, but from the larger group with intermediate risk.
Different studies have:
- used different inclusion and exclusion criteria
- defined low-trauma fractures in different ways
- ascertained different combinations of fractures as the outcome
Based on proximal femur BMD from a population-based cohort study of 616 postmenopausal Australian women followed for 5.6 years:
- 26.9% of radiologically confirmed fractures arose from women with osteoporosis
- 73.1% from women without osteoporosis (56.5% from women with osteopenia and 16.6% from women with normal BMD measured at the total hip)
Similarly, in a cohort study of 149,524 postmenopausal white women enrolled in National Osteoporosis Risk Assessment (NORA) from primary care practices in the United States and followed for 12 months after baseline assessment using BMD measurements obtained from a variety of peripheral devices (heel, finger, or forearm):
- 18% of self-reported fractures arose from women with osteoporosis
- 82% from women without osteoporosis (52% from women with osteopenia and 30% from women with normal BMD)
The NORA data excluded those with a historyof known osteoporosis or anti-fracture therapyand this may explain the difference in the proportion of fractures arising from each BMD category between the Australian and U.S. studies.
Furthermore, the prevalence of osteoporosis and osteopenia varies depending on:
- the device
- the site of BMD measurement
- the reference population used to define T-scores
Same-site differences exist, not only between machines from the same manufacturer, but also across devices made by different manufacturers.
Peripheral devices generate T-scores that may differ from those derived using hip or spine DXA, and the choice of reference population impacts on the BMD cut-points for identifying osteopenia and osteoporosis.
The Geelong Osteoporosis Study (GOS) data used proximal femur BMD because of the well-recognized influence of age-related artifacts on spine BMD measurements.
However, despite these methodological limitations, greater numbers of fractures are consistently shown to arise in women with normal or osteopenic BMD.
This may simply be a consequence of larger numbers of women at risk of fracture in these groups.
However, the risk for fracture is multifactorial. Many clinical risk factors for fracture operate through reduced BMD; however, othersact independent of BMD.
Increasing age contributes independently to the risk of fracture.
For the same BMD, the risk of fracture varies by a factor of 8 to 10 between women aged:
- less than 45 years
- 80 years and older
Even though the majority of individuals who sustain a fragility fracture do not have a prevalent fracture (this proportion is 75% among women with osteopenia), a prior fracture independently doubles the risk of subsequent fracture.
Women with osteopenia and a prevalent fracture are at comparable risk to those with osteoporosis on BMD criteria.
Low body mass index is recognized as a risk factor for fracture that is essentially independent of age and sex, but dependent on BMD.
Falls independently increase the risk of fracture.
Fracture Risk Assessment
Various models for predicting fracture have been developed that involve BMD in conjunction with clinical risk factors with an aim of improving risk stratification, particularly within the large group with moderate bone deficits categorized as osteopenia.
The World Health Organization's collaborating center developed the Fracture Risk Assessment Tool (FRAX) algorithm as a tool based on clinical risk factors, with and without BMD, using primary data from multi-national prospective cohort studies.
The FRAX estimates 10-year probability of hip fractures and major osteoporotic fractures, including fractures of the:
- hip
- spine
- humerus (a long bone in the upper arm or forelimb)
- wrist
In Australia, data from two population-based studies independently combined BMD and clinical risk factors to generate fracture risk assessment tools.
The said two studies are:
- GOS (Graduate Outcomes Survey), which created the GOS Fracture Risk (FRISK) Score
- DOES (Dubbo Osteoporosis Epidemiology Study), which created the Garvan algorithm
The GOS FRISK estimated 10-year probability of low-trauma fractures at the:
- hip
- spine
- forearm
- humerus
The Garvan predicted 5-year and 10-year probability of fragility fractures of the:
| clavicle | pelvis |
| hand | scapula |
| hip | spine |
| humerus | sternum |
| lower limb | wrist |
The FRAX includes multiple clinical risk factors, whereas both the GOS FRISK and Garvan utilize fewer risk factors.
The FRAX did not include falls because these data were not consistently collected across the multiple population-based studies from which the data were derived.
The purpose of developing such models is to provide clinically useful tools to better identify, with high sensitivity and specificity, individuals in the population who are at greatest risk for fracture.
Bone Microarchitecture And Structure
The observation that age and previous fracture independently increase the risk for fracture is consistent with the notion that increasing age and fragility fracture are markers for greater material or structural deterioration in bone, not quantified by BMD.
Bone morphology and microarchitecture contribute to the breaking strength of bone.
To be strong, bones need to be stiff enough to withstand deformation under loading, yet adequately elastic to absorb energy during compression and tension.
Recently developed technologies for assessing bone structure include high-resolution peripheral quantitative computed tomography (pQCT) and magnetic resonance imaging that have the advantage of simultaneously assessing trabecular and cortical components of bone separately, in addition to geometric characteristics of the peripheral skeleton.
In a matched case–control study of postmenopausal French women, 101 cases with fragility fracture over 13 years of follow-up were matched with fracture-free controls.
Vertebral and nonvertebral fractures were associated with low volumetric BMD and structural deterioration of trabecular and cortical bone as assessed by high-resolution pQCT at the distal radius and tibia, independent of areal BMD.
Cases had decreased:
- trabecular volume
- cortical thickness
- trabecular number
- trabecular thickness
Similarly, according to another study using high-resolution pQCT, compared to osteopenic women, osteoporotic women had:
- lower density
- cortical thickness
- increased trabecular separation
Among osteopenic women, those with fracture had lower trabecular density and more heterogeneous trabecular distribution.
These women were defined as having osteoporosis or osteopenia based on measurements of BMD at the lumbar spine or proximal femur.
The lower T-score was used to categorize subjects.
A proportion of those with BMD in the osteopenic range at the lumbar spine alone are likely to have had osteoporosis with the BMD measurement being spuriously increased by artifact.
The apparent greater micro-architectural deterioration among those women with osteopenia and fracture may therefore have been related to miscategorization.
The pQCT assessment of the ultradistal (UD) radius in the United States shows that the structural basis for the observed decrease in trabecular volume differs between men and women.
With aging:
- women undergo loss of trabeculae with an increase in trabecular separation
- men start with thicker trabeculae and experience less age-related microstructural damage
Because decreases in trabecular numbers substantially affect bone strength, this finding may explain, at least in part, the protection men have against age-related increases in distal forearm fractures.
More recent findings suggest that development of intracortical porosity may play an important role in compromising bone strength and that this could explain the high proportion of non-vertebral fractures that occur with aging at predominantly cortical sites.
In an Australian study of 185 female twin pairs aged 40-61 years, postmenopausal women were found to have higher levels of remodeling markers that were associated with larger intracortical surface area rather than with the progressively diminishing trabecular surface area.
Identification of intracortical, endocortical, and trabecular bone surface area are beyond the resolution of contemporary DXA analysis and are, therefore, not accounted for using BMD from DXA.
Conclusion
Fragility fractures pose a considerable health burden to the community.
Effective strategies to reduce the burden of fractures depend on the development of preventive measures to target lifestyle or pharmacological interventions, based on identification of individuals at risk.
The burden of fractures arises, not from the relative few with severely low BMD identified as osteoporosis, but from those with mild to moderate bone deficits.
Individuals with osteopenia are commonly not treated because there is a lack of data relating to anti-fracture therapies in this group and, based on post hoc analyses from osteoporosis clinical trials, the numbers needed to treat are too large to be economically feasible if the whole group is to be considered.
Yet, over half of the fractures in the population arise from this group.
Those at highest risk for fracture within this group need to be identified and evidence-based treatment strategies developed to reduce the public health burden of fractures.
Improved risk stratification may be achieved by quantifying factors that contribute to bone strength, such as:
- bone morphology
- microarchitecture
They are properties beyond the resolution of conventional densitometry by DXA.
It needs to be demonstrated that such predictors of risk are amenable to reduction with osteoporosis therapies and that anti-fracture treatment reduces fracture risk before recommendations are deemed appropriate.
Non-bone risk factors, that are amenable to modification, also need to be considered.
Information about osteopenia and its correlation with low bone mass and fractures will always be helpful.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles